ARTÍCULO |
Mind lines against guidelines in treatment of malaria. A Comparative Cross Sectional Study from Pakistan
Madeeha Malik*, Mohamed Azmi Ahmad Hassali, Asrul Akmal Shafie, Azhar Hussain.
Discipline of Social and Administrative Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, 11800 Minden, Penang, Malaysia.
e-mail: mady_sweet1@yahoo.com
Recibido el 1 de septiembre de 2012
An. R. Acad. Farm. 78, 4, 2012, 499-510
abstract
A comparative, cross-sectional study was designed to assess the adherence of prescribers with national standard treatment guidelines for malaria in all the twenty public and private tertiary healthcare facilities in the two cities of Pakistan. A total of 600 patient encounters were assessed with the national standard treatment regimen for malaria. No significant difference at (p ≤ 0.05) was observed among adherence of prescribers having different designations and levels of experience with standard treatment regimen for malaria in the two cities. The results of the present study showed low adherence of prescribers with standard treatment regimen for malaria in Pakistan. |
Palabras clave: Adherence; Malaria; Pakistan; Standard treatment guidelines.
resumen
Juicio sobre la adherencia a las directrices de tratamiento de la malaria. Un estudio transversal comparativo en Pakistán
Se diseĖó un estudio transversal comparativo para evaluar la adherencia de los prescriptores a las pautas estándar nacionales de tratamiento de la malaria, en veinte instalaciones sanitarias terciarias, públicas y privadas, de dos ciudades de Pakistán. Se evaluaron un total de 600 encuestas a pacientes sometidos al régimen estándar nacional de tratamiento contra la malaria. No se observó diferencia significativa alguna (a nivel de p ≤ 0.05) sobre la adherencia de prescriptores con diferentes niveles de experiencia con el régimen de tratamiento estándar para la malaria en las dos ciudades. Los resultados del presente estudio mostraron baja adhesión de los prescriptores al régimen de tratamiento estándar para la malaria en Pakistán. |
Keywords: Pautas de tratamiento estándar; Adherencia; Malaria; Pakistán.
1. introduction
The rational use of drugs demands that appropriate drugs must be prescribed and available at the right time and at an affordable price to the patients. Prescribing patterns might influence the effectiveness of treatment and the control of disease. Inadequate, excessive or incorrect prescribing practices are most likely to be the commonest forms of irrational prescribing habits. Development of resistance to antibiotics, ineffective treatment, adverse effects, drug dependence and economic burden to the patient and society due to irrational prescribing practices are the major dilemma of present medical practice in case of malaria (1).
Rational prescribing requires that the prescribers adhere to standard treatment guidelines to facilitate a constant, therapeutically effective and economically efficient use of drugs. This greatly enhance the compliance of patients and outcome of therapy (2). But most of the medical practitioners in developing countries including Pakistan are prone to practice their own protocols to treat malaria rather than adhering to standard regimens. Promoting the rational use of drugs remains a major challenge.
Standard treatment guidelines are one of the tools to support effective clinical practice and promotion of rational use of drugs. These guidelines must be implemented and the monitoring of case management according to these guidelines must be evaluated (3). Standard treatment guidelines for Malaria have been formulated and introduced in 2005 through collaborative efforts of directorate of malaria control, WHO and technical core group in Pakistan (4). Chloroquine is recommended as first line drug in the treatment of all types of malaria. Sulfadoxine/pyrimethamine and artemether/lumefentrine are recommended as first line drugs for treatment of confirmed cases of Plasmodium.falciparum. Chloroquine along with premaquine combination is used as anti relapse therapeutic agents in case of Plasmodium.vivax (4) (Table 1).
Table 1.- Standard treatment guidelines for malaria in Pakistan.
Anti-malarial drugs |
Dosage form |
Comments |
Chloroquine is first choice of drug in all cases of malaria when type not confirmed through laboratory test for empiriacl therapy |
||
Standard treatment regimen for P.vivax |
||
Chloroquine + primaquine |
Tablets |
Chloroquine 25mg/kg for 3days + primaquine 0.25mg/kg O.D for 14 days. |
Primaquine |
Tablets |
0.75mg/kg body weight once a week for 8weeks. |
Standard treatment regimen for confirmed cases of P.falciparum |
||
Artemether +lumefantrine |
Tablets |
Artemether 20mg +lumefantrine 120mg two doses per day for 3 days. |
Artesunate +tetracycline |
Tablets |
Artesunate 20mg /kg O.D +tetracycline 4mg/kg Q.I.D for 7days. |
Dihydroartemisinin+ piperaquine |
Tablets |
Dihydroartemisinin 4mg/kg/day +piperaquine 18mg/kg/day for 3days. |
Single dose piperaquine |
Tablets |
(0.75 mg/kg) to ACT treatment |
*Directorate of Malaria Control and WHO, National treatment guidelines for malaria. 2005
Although, standard treatment guidelines are available in the country, still prescribing and dispensing practices are not up to the desired standards in public and private healthcare facilities in Pakistan (5).
There is lack of research on evaluating the adherence of prescribing practices with these standard treatment guidelines, which in turn has strong influence on malaria treatment practices (6). Therefore, the main objective of the present study was to assess the adherence of prescribers with national standard treatment guidelines for malaria in the two cities of Pakistan; Islamabad (national capital) and in its twin city Rawalpindi.
The study will provide baseline data regarding adherence of prescribers with standard treatment guidelines, which can serve as a basis for potential areas for intervention to implement the standard treatment guidelines effectively to improve rational drug use in the healthcare system.
2. MATERIALs and MeThODS
Study design
A comparative, cross-sectional study was designed to evaluate the case records of patients from October 2010- 2011 including (daily registers, medical records, prescriptions, patient-held records) treated for malaria in public and private tertiary healthcare facilities in the twin cities, namely Islamabad (federal capital) and Rawalpindi.
Study tool
The case records were collected from the male and female medicine wards and out-patient departments (OPD) of the healthcare facilities. A pre-validated tool i.e. WHO prescribing indicator form was used to collect data regarding current prescribing practices for the treatment of malaria(7).
The prescribing form included five core indicators such as % of encounters having diagnosis, average number of drugs per encounter, % average number of antibiotics and injections prescribed per encounter and % of drugs prescribed by generic names. Beside this few additional indices such as demographics of patient, type of drug combinations prescribed and availability of standard treatment guidelines in the healthcare facilities were also assessed.
Prescriptions were also assessed for the prescribed anti-malarial drugs, their doses, strengths, frequencies and durations of use to check whether if they followed national standard treatment regimen or not. The minimum requirement for the adherence of prescriptions with standard treatment regimen was elaborated and transformed into measurable adherence indicators scale. The scale included five indicators including correct prescribing of right anti-malarial drug, its dose, strength, frequency and duration of use. The composite score for the scale was 5-10 and lower score referred to better adherence with the standard treatment regimen.
Data collection was planned and permission for survey was obtained from relevant district health officers (DHO) and Medical superintendents (MS) of respective healthcare facilities. The study was also approved by Malaria Control Program, Ministry of Health, Government of Pakistan.
Sampling of facilities and patient encounters
Keeping in view the federal administrative and regulatory structure of the country and due to location and operation of Malaria Control Program in the capital city, two main cities of Pakistan namely Islamabad and Rawalpindi were selected for the study. The public healthcare facilities providing services at provincial and district levels are categorized as: primary level health care facilities (basic health units, rural health centers, mother & child health centers, TB clinics and dispensaries), secondary level health care facilities (tehsil headquarter hospitals and district head quarter hospitals) and tertiary level health care facilities (tertiary hospitals, post graduate medical institutes, teaching hospitals). All the tertiary healthcare facilities have a primary section for treating common disease including malaria.
Cases are referred from lower to higher level depending on severity of problem and available infrastructure (8). The study population included all the public and private tertiary health care facilities treating malaria in Islamabad and Rawalpindi. A list of all the public and private tertiary healthcare facilities was obtained from respective District Health Offices. All the 20 public and private tertiary healthcare facilities were selected for the study and the sample size was Islamabad (n =10, 5 each public and private healthcare facilities) and Rawalpindi (n =10, 5 each public and private healthcare facilities).
For assessing the prescribing practices in each facility, thirty patients treated for malaria by the prescribers over the last one year were reviewed (7).
A total of 600 patient encounters i.e. 300 from each sector (public and private) healthcare facilities situated in both cities were collected randomly from daily registers, medical records, prescriptions, patient-held records. At least two patients encounter per month during the low season (October till April) and four patients encounter per month during the high season (May till September) for malaria were selected.
As there is no trend of laboratory confirmation of malaria in Pakistan all the prescriptions with diagnosis of malaria, anti-malarial drugs and tests of malaria parasite results were included in the sample. Plasmodium vivax is common in Rawalpindi and Islamabad so the adherence of prescribers with standard treatment regimen for P.vivax was assessed.
Interview of the head of the outpatient department on recommended current prescribing practices in the healthcare facilities were recorded and applied to all encounters where records were missing (9). Prescriptions without the name of the prescriber and folder without patient’s information were excluded. The prescribers were identified from patient’s prescriptions and information regarding their designation and experience was recorded.
Data collection and analysis
Data was collected by the principal investigator along with two teams comprised of five trained data collectors in each team trained by the group of experts including principal investigator (9).
The data collectors were trained students of the final year Doctor of Pharmacy program who tallied data with standard treatment regimen. Data were coded and analyzed using statistical software SPSS version 16. Descriptive statistics (frequencies and percentages) were used to describe trends in the current prescribing practices. Kruskal-Wallis test (p ≤ 0.05) was used to compare the adherence of prescribers with standard malaria regimen having different designations and level of experiences. While Mann Whitney test (p ≤ 0.05) was used to compare the adherence of prescribers with standard treatment regimen for malaria practicing in public and private healthcare facilities in the two cities.
3. RESULTS
A total of 600 malaria cases were collected and analyzed. Out of 600 encounters, 50 % (n=300) were collected from public and 50 % (n=300) were from private tertiary healthcare facilities.
The mean age of the malaria patients in the encounters was 35.00 years (Ī 14.04), ranging from 20 to 60 years while 68.3% (n=410) of the patients were males and remaining 31.7% (n=190) were females.
Of the total prescriptions, 34.3 % (n= 206) were prescribed by house officers (fresh MBBS graduate acquiring training in medical fertinity), 57.7 % (n = 346) were by medical officers (Medical graduate with at least experience of more than one year) and remaining 8 % (n = 48) were by specialists (Medical graduate with expertise in a specific field of medical fertinity).
It was observed that 20.2 % (n = 121) of the prescribers had working experience of less than one year, 40.7 % (n = 244) had working experience of 1-5 years, 23.7 % (n = 142) had working experience of 6-10 years and 15.5 % (n = 93) had working experience of more than 10 years. Of the total prescribers, 85 % (n= 510) were not aware regarding national standard treatment guidelines for malaria, 90 % (n = 540) have never seen them in their health facilities for reference and 98.3 % (n = 590) had never received any training on standard treatment guidelines for malaria (Table 2).
The mean number of drugs per encounter was 2.37 (Ī 0.557), ranging from 1 to 5 drugs per encounter while mean number of antibiotics and injections per encounter were 0.32 (Ī 0.513) and 0.23 (Ī 0.470), ranging from 1 to 2 antibiotics and injections per encounter respectively. Diagnosis was written on 37.2% (n = 226), of the prescriptions while results of Malarial Parasite (MP) test was mentioned in only 9.2 % (n= 55) of the cases. In 29.1% (n= 175) of the cases antibiotics and in 21.6% (n= 126) of the cases injections were prescribed.
Drugs were prescribed by their generic names in only 3% (n= 18) of the cases. While dose of the anti-malarial drugs was not calculated as per patient body weight in any of the encounters. The most commonly prescribed anti-malarial drugs were chloroquine phosphate 11 % (n= 66), artemether/lumefantrine 17.4 % (n= 321), artemether 17.4 % (n= 104), sulphadoxine/pyremethamine 10.5% (n= 63) and amidaquine HCl 7.7 % (n= 46) (Table 3).
Table 2.- Demographics.
Parameter |
F (%) |
Designation Specialists Medical officer House office |
48 (8) 346 (57.8) 206 (34.3) |
Experience Less than one year 1-5 years 6-10 years More than 10 years |
121 (20.2) 244 (40.7) 142 (23.7) 93 (15.5) |
Prescribers aware of malaria STGs Yes No |
90 (15) 510 (85) |
Prescribers received any training on malaria STGs Yes No |
60 (10) 540 (90) |
Availability of STG for malaria in health facilities Yes No |
10 (1.7) 590 (98.3) |
Table 3.- Prescribing trends in tertiary healthcare facilities.
Indicator |
Prescriptions n = 600 F (%) |
Diagnosis written on prescriptions |
226 (37.7 %) |
Results of MP test on prescriptions |
55 (9.2 %) |
Antibiotics prescribed |
175 (29.2 %) |
Injections prescribed |
126 (21 %) |
Anti-pyretic prescribed |
554 (92.4 %) |
Prescribing by generic name |
18 (3 %) |
Chloroquine phosphate prescribed |
66 (11 %) |
Artemether/lumefentraine prescribed |
321 (53.5 %) |
Artemether prescribed |
104 (17.3 %) |
Sulphadoxine/pyremethamine prescribed |
63 (10.5 %) |
Amodiaquine HCl prescribed |
46 (7.7 %) |
Out of 600 encounters, correct anti-malarial drugs were prescribed in 11 % (n= 66) of the cases, correct dose of anti-malarial drugs used were given in 10.1 % (n= 61) of the cases while correct strength of anti-malarial drugs used was prescribed in 9 % (n= 54), correct frequency of the drugs used in 9.2 % (n= 55) and correct duration of drugs used in 9 % (n= 54) of the cases respectively.
A detail description of prescriptions prescribed according to malaria STGs in public and private healthcare facilities in the two cities is given in (Table 4).
Table 4.- Adherence of prescriptions with standard treatment
guidelines for malaria in public and private tertiary healthcare facilities in
the two cities.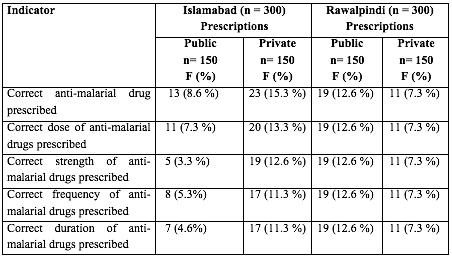
No significant difference (p ≤ 0.05) was observed among adherence of prescriptions with standard treatment regimen for malaria in public and private healthcare facilities in the two cities (Table 5).
No significant difference (p ≤ 0.05) was observed among adherence of
prescribers having different designations and levels of experience with
standard treatment regimen for malaria (Table 6).
Table 5.- Comparison of adherence of prescriptions with standard treatment guidelines for malaria prescribed in public and private tertiary healthcare facilities in the two cities.
Variables |
Adherence of prescriptions with standard treatment guidelines for malaria |
|||
n |
Median |
U |
P value |
|
Cities |
Islamabad = 300 Rawalpindi = 300 |
Islamabad = 10 Rawalpindi = 10 |
4.440 |
0.300 |
Sector |
Public = 300 Private = 300 |
Public = 10 Private = 10 |
4.468 |
0.389 |
Table 6.- Comparison of adherence of prescribers with standard treatment guidelines for malaria having different level of experience and designations working in tertiary healthcare facilities.
Variables |
Adherence of prescribers with standard treatment guidelines for malaria |
|||
n |
Median |
H |
P value |
|
Experience |
Less than 1 year = 121 1-5 years = 244 6-10 years = 142 More than 10 years = 93 |
Less than 1 year = 10 1-5 years = 10 6-10 years = 10 More than 10 years = 10 |
6.482 |
0.090 |
Designation |
House officer = 206 Medical officer = 346 Specialist = 48 |
House officer = 10 Medical officer = 10 Specialist = 10 |
1.213 |
0.560 |
4. discusSion
Irrational use of drugs is a major challenge faced by the healthcare systems of developing countries. Prescribing of anti-malarial drugs to patients without evidence of malaria parasitaemia and the recurrent absence of treatment for alternative causes of disease is a common practice at healthcare facilities in these countries (10).
Laboratory diagnosis can improve the treatment of malaria, but the results of the present study showed that only few facilities were offering any laboratory diagnostic services for the confirmation of malaria before prescribing anti-malarial drugs to the patients. However, it was observed that prescribing of anti-malarial drugs after laboratory confirmation only decreased significantly the total number of prescriptions in Malawi (11).
Antibiotics are usually not preferred in the treatment of malaria and do not conform to the treatment guidelines. But prescribing of anti-malarial drugs along with an antibiotic and an antipyretic was seen as a common practice at both public and private healthcare facilities.
The results of the present study are in line with another study indicating overuse of antibiotics and injections promoting irrational drug use and higher rate of emergence of resistance of anti-malarial drugs (12). Dose of the anti-malarial drugs was not calculated as per patient body weight and drugs were mostly being prescribed by their brand names. The overall low generic prescribing observed was comparable to the results of the other studies conducted in Nigeria and Nepal (13, 14).
Chloroquine is usually the most commonly prescribed oral antimalarial drug in most of the countries as compared to quinine and other anti-malarial drugs due to its continuous availability, affordable price or an established pattern by which most doctors treat uncomplicated malaria initially by giving chloroquine, followed by oral quinine for non-responding cases. Similar pattern was followed in healthcare facilities in Nigeria (15). Although, Chloroquine is recommended as first line drug in the treatment of all types of malaria while Sulfadoxine/pyrimethamine and artemether/lumefentraine are only recommended as first line drugs for confirmed cases of Plasmodium falciparum in national standard treatment guidelines of Pakistan.
The prevalence of P. vivax is more common in Punjab while P. falciparum is more frequently seen in Baluchistan and Sindh (4). But the results of the present study showed significant use of artemisinin based combination therapy for the treatment of malaria in Punjab although most of them were aware of the fact that P. vivax is more common in Punjab.
Rational prescribing requires that prescribers follow a standard process of prescribing and in accordance with standard treatment guidelines. High rate of inappropriate prescriptions for treating malaria are mostly due to lack or incorrect doses, frequency, dosages and duration of treatment (15).
The result of the present study showed poor adherence of prescribers with the standard treatment guidelines for malaria. Prescribers having different designations and levels of experience working in public or private sector were not adhering to standard treatment guidelines. Most of the prescribers were unaware of the standard treatment guidelines and have never received any training on them.
The standard treatment guidelines were not available in any of the healthcare facilities. This clearly reflects on the poor implementation of standard treatment guidelines for malaria in the country. However, adherence of prescribers with the standard treatment guidelines was significantly improved after receiving training on them in Nigeria (16).
5. Conclusion
The present study revealed that despite the availability of standard treatment guidelines in the country, the pattern of prescription in terms of adherence and rationality remains poor.
There is an urgent need to implement standard treatment guidelines and develop ways and means to ensure their availability and adherence of prescribers to them in the healthcare facilities. Malaria control program must play its role more effectively and should arrange special training programs for the prescribers on standard treatment guidelines.
Regular continuing medical education (CME) must be made mandatory for the prescribers to attend, so as to update their knowledge. A check on the influence of pharmaceutical companies and their representatives needs to be maintained in health institutions, to minimize their influence on the drug prescription. All these measures would go a long way in provision of more rational, economical, and effective treatment to the patients and control of the disease.
5. REFERENCeS
1. Juncosa, B., (2008) Antibiotic Resistance: Blame It on Lifesaving Malaria Drug?, Scientific American., 2008, July,21
2. Chukwuani, C., Onifade, M. and Sumonu K.(2002). Survey of drug use practices and antibiotic prescribing pattern at a general hospital in Nigeria. Pharmacy World & Science, 24(5): 188-195.
3. Le Grand, A., Hogerzeil, H.V. and Haaijer-Ruskamp, F.M. (1999) Intervention research in rational use of drugs: a review. Health Policy and Planning,. 14(2): 89.
4. Directorate of Malaria Control and WHO (2005) National treatment guidelines for malaria,.
5. Nizamani, A., Kalar, N.A. and. Khushk, I.A (2006) Burden of malaria in Sindh, Pakistan: a two years surveillance report. J. Liaqat Uni. Med. Health Sci., 5: 76-83
6. Meremikwu,M., Okomo,U., Nwachukwu, Ch., Oyo-ItaA., Eke-Njoku,J., Okebe1, J., Oyo-Ita,E. and Garner, P. ( 2007) Antimalarial drug prescribing practice in private and public health facilities in South-east Nigeria: a descriptive study. Malar J. 6(55). doi:10.1186/1475-2875-6-55
7. World Health Organization, How to Investigate Drug Use in Health Facilities: Selected Drug Use Indicators: Action Programme on Essential Drugs 1993: World Health Organization.
8. Ghaffar, A., Kazi, B.M. and Salman, M. (2000) Health care systems in transition III. Pakistan, Part I. An overview of the health care system in Pakistan. Journal of Public Health, 22(1): 38-42
9. Rational Pharmaceutical Management Plus Program, Pharmaceutical Management for Malaria, USAD, Editor 2004, U.S. Agency for International Development: USA.
10. Obinna, O., Kaur,H., Dike, E., Shu,E., Uzochukwu,B., Hanson,K., Okoye,V. and Okonkwo,P. et al., (2009). Malaria treatment perceptions, practices and influences on provider behaviour: comparing hospitals and non-hospitals in south-east Nigeria. Mal.,J., 8: 246-. doi:10.1186/1475-2875-8-22
11. Chitaka, R.,. Khare, A.K and Brickling, C. (1998). Prescribing policy for antimalarials. . African Health, 20(2): 2-5.
12. Das, N., Baloch H. Khan, A. NBadini, Z. A. Parkash,J. et al., (2001). Prescribing practices of consultants at Karachi, Pakistan. Journal-Pakistan Medical Association, 51(2): 74-77.
13. Elhassan, A.M.S.A.(1999). Prescribing and dispensing practice at NGO, govemment.and private clinics in Nepalguni municipality. Nepal INRUD News 9: 25-26.
14. Igboeli, N.U., Ukwe, C.V. and Ekwunife, O.I. (2010). Increasing use of artemisinin-based combination therapy for treatment of malaria infection in Nigerian hospitals. Pharmacy Practice (Internet), 8(4): 243-249.
15. Yousif, M.A. and Adeel, A.A. (2000). Antimalarials prescribing patterns in Gezira State: precepts and practices. Eastern Mediterranean Health Journal, 15(5/6):. 939-947.
16. Adibe, M.O.(2010). Predictors to adherence to national anti-malarial treatment guidelines in some Nigerian hospitals. Inter.J Drug Development and Research, 2(3): 545-554.